Polycystic Ovarian Syndrome (PCOS) is a complex condition. Too often, women and their health care providers don’t recognise the connection between PCOS and gut health.
While physicians are becoming more familiar with PCOS, the diagnosis is often missed. The standard fix to period problems or hormonal acne is to be started on birth control pills. This often masks the condition and can worsen gut health. It is often only when you decide to discontinue oral contraception to become pregnant that there is a deeper dive into the symptoms if they return.
PCOS is a significant risk factor for numerous chronic diseases beyond the emotional distress of hormonal acne or irregular periods and other symptoms.
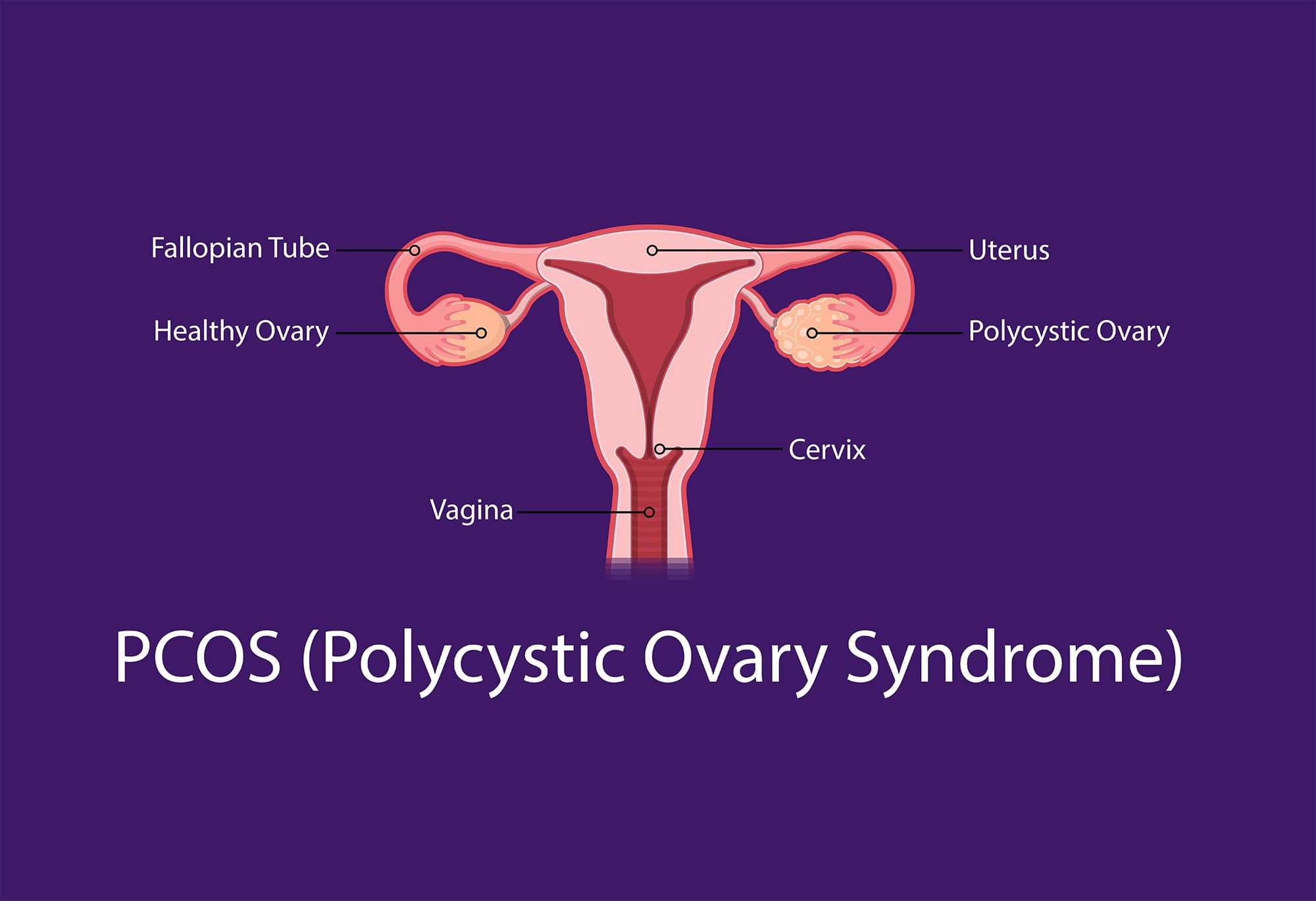
What is PCOS?
PCOS is often characterised by high levels of male hormones and an imbalance of female hormones. It is one of the most common causes of infertility due to the direct interference with ovulation.
High male hormones can cause symptoms such as weight gain, sleep apnoea, oily skin or acne, irregular or absent periods, hair loss or hair thinning, coarse body hair growth, and difficulty falling pregnant.
Many women with PCOS also have problems with insulin resistance which can lead to Type 2 Diabetes and weight gain (especially around the mid-section). Weight gain and insulin resistance can also result in higher triglycerides as well as high LDL cholesterol (bad cholesterol) and low HDL cholesterol (good cholesterol).
Although the name suggests that this condition is associated with the ovaries…and you would rightly assume that it is specifically a hormonal condition, it actually has a grounding in metabolic health, inflammation, and adrenal function. Confusing? We know. The good news is that PCOS can be significantly lessened or even reversed with the proper diet, lifestyle, and nutritional support.
The Types of PCOS
There are four types of PCOS. Although they appear straightforward, the diagnosis should be made by a health care professional who can interpret pathology results. The diagnosis requires numerous clinical testing and, in some cases, by elimination of other more serious issues. This is very frustrating for the individual, but all possibilities need to be explored.
1. Insulin Resistant PCOS
This is one of the most common types of PCOS and results from elevated insulin levels in the body. You may hear this being referred to as metabolic syndrome or pre-diabetes.
Insulin resistance occurs when the cells in your body stop responding to insulin. Insulin’s main role is to reduce our blood sugar (glucose). It does this by ‘opening’ the cell and allowing glucose in which is necessary for many cells to function. Think of it as a lock and key situation. Insulin is the key that unlocks the cell that allows fuel to enter the cell.
When insulin can’t do its job, there is an increase in blood glucose levels. This is because the glucose (fuel for the cell) can’t get in to do its job. The pancreas is alerted and cranks up the production of insulin…thinking that there is not enough insulin to get the glucose into the cells.
This increase in circulating insulin triggers the production of androgens in women and interferes with ovulation, which leads to all the symptoms mentioned above.
Other symptoms common with this type of PCOS include fatigue, brain fog, frequent thirst, and weight gain around the middle. To diagnose this type of PCOS, you will need to test your insulin levels.
2. Post Pill PCOS
This occurs in some individuals after they stop taking the oral contraceptive pill. Symptoms usually manifest as acne, irregular periods, and excessive hair growth.
Not all oral contraceptives will trigger this sort of reaction. It usually involves oral contraceptive pills with synthetic progestins in the formulation.
The good news about this type of PCOS is that the symptoms usually decrease 3-6 months after stopping the pill. However, it can take longer. The focus here should be on the temporary nature of the problem.
3. Adrenal PCOS
This type of PCOS is found in about 20-30% of those diagnosed (Yildiz & Azziz, 2007) and is primarily due to an abnormal stress response. It is where DHEA-S (a type of androgen from the adrenal gland) is elevated. Typically, other types of androgens, such as testosterone, are not seen in the pathology reports.
However, this type of androgen is not tested regularly, so if you are concerned, you may need to ask for this level to be done or see a specialist, like an endocrinologist.
4. Inflammatory PCOS
This type of PCOS is caused by chronic inflammation in the body. The inflammation triggers the ovaries to produce excess testosterone. The hallmark symptoms tend to be headaches, joint pain, unexplained fatigue, and skin issues. Your blood results will usually show an elevated C reactive protein and occasional increases in fasting glucose and insulin…but not always.
What causes PCOS?
You will not want to hear this, but the cause isn’t clear. It is believed there is an interplay between genetics, stress, alterations in hormone secretions, inflammation, autoimmunity, and gut dysbiosis (Bednarska & Siejka, 2017).
Although there is a complicated debate over what constitutes a diagnosis of PCOS, there are two biochemical factors that are always agreed upon. These are the presence of chronic inflammation and insulin resistance (Tremellen & Pearce, 2012).
One of the most likely scenarios is that certain strains of harmful bacteria are well-known stimulants of inflammation. This increases the permeability of the intestinal walls allowing inflammatory chemicals to be released into the bloodstream.
This can lead to insulin receptors’ inactivation, preventing insulin from opening the target cell for fuel. This increase in blood insulin levels and the elevation of inflammatory factors, can trigger a rise in androgen production (Tremellen & Pearce, 2012).
Interesting facts with relation to the gut that have been discovered about PCOS:
- Women with the condition have a less diverse microbiota compared to controls (Pedro, et al., 2018),.
- Gut microbiota plays a role in regulating androgens (Collden, et al., 2019).
- Women with PCOS have a higher level of certain harmful bacteria strains that positively correlate with BMI and testosterone (Guo, et al., 2016).
- Poor gut and poor liver function increase the reabsorption of oestrogen which worsens symptoms – Remember testosterone reduces ovulation! This means when we don’t ovulate, we don’t produce progesterone. When we don’t produce progesterone we become oestrogen dominant. This perpetuates the cycle – unhappy gut = unhappy hormones!
What can I do to help myself if I have PCOS?
There are a range of invasive and non-invasive treatments offered by mainstream medicine; however, you will still need to take control of the situation and do some of the work yourself.
While this may seem like an uphill battle when you are going through it, there are things that you can do to improve gut health, balance the intestinal microbiome, and help you manage your PCOS. Sometimes dietary factors alone are not enough, so it will be beneficial to look at your entire lifestyle. This will produce an environment for beneficial bacteria to thrive (Rowland, et al., 2017).
Prebiotics
Prebiotics feed the beneficial bacteria in your gut. It is a fibre resistant to digestive enzymes so is not absorbed in the small intestine. It makes its way to the colon, where it stimulates the growth and activity of beneficial gut bacteria – much like sending the probiotics a packed lunch! It is their ‘superpower food.’
Foods rich in prebiotics are garlic, onion, asparagus, artichokes, and apples. And, of course, Gut Performance™ is the perfect prebiotic supermix. With just one scoop a day, it is your ready-made daily dose to feed, fertilise and sustain good gut bacteria and health.
Probiotics
These are friendly bacteria that help restore the balance and composition of your gut flora. You can obtain probiotics in natural food sources such as fermented foods like sauerkraut, kimchi, or kombucha.
You can also supplement through capsule form, but ‘buyer beware.’ Not all supplements are created equal. It depends on how they are prepared, the strains present, and even how they are stored.
Adding additional beneficial bacteria into our gut system is always good when we are depleted. It is best to work closely with a health care practitioner to prescribe the correct strain for the correct condition and who have access to quality products. Otherwise, you will be pooping your money down the toilet – literally!
Antioxidants and Anti-inflammatory Foods
Poor gut health significantly contributes to increased inflammation in the body, and the microbiome plays a significant role in the regulation of inflammation.
Now you know that PCOS is associated with chronic low-grade inflammation. Eating foods that help reduce overall inflammation is helpful. The foods you need to choose should be rich in antioxidants such as turmeric, berries, tomatoes, cruciferous vegetables, meat and fish high in omega 3 fatty acids such as mackerel and sardines – always try to go for the smaller fish!
Gut Performance™ is also jam-packed with antioxidants that directly reduce gut inflammation. Use the Gut Performance™ + Collagen, and you will be giving your gut the extra love it needs to repair any excess damage. Fun fact – Not only is collagen great for our skin, joints, hair etc, it also works wonders to help repair the gut lining!
Cut down on Sugars
Excessive sugar promotes inflammation in the body and contributes directly to dysbiosis in the intestinal tract. Sugar is hidden in all our processed foods, even those you think are healthy. Just look at the labels on your kombucha, sweetened teas, condiments, and sports drinks.
We are not saying completely cut out sugars, but enjoy them in moderation and opt for the natural variety. Also, watch out for artificial sweeteners, they may be promoted as a healthier option, however, there is a growing body of evidence to suggest that some may alter the gut microbiome (Ruiz-Ojeda, Plaza-Diaz, Saez-Lara, & Gil, 2019).
Move Your Body
Moving your body daily is incredibly beneficial for your overall physical and mental health. Specifically, for people who suffer from PCOS, it boosts insulin sensitivity, increases endorphins, promotes better sleep, lowers your risk of heart disease, helps to regulate hormones, and encourages weight loss.
Stress Less
We all know that prolonged stress exacerbates digestive issues. It alters the gut microbiome, makes the lining of the intestinal wall more permeable, and impacts sensitivity and motility (a term used to describe the contraction of the muscles that mix and propel contents in the gastrointestinal (GI) tract).
You need to keep in mind that stress management looks different for every individual. But some places to start can be yoga, meditation, walking, and getting out in nature.
Get Some Shut-Eye
Lack of sleep is a massive stressor on the body, impacting the gut in more than one way. The result is often dysbiosis and changes to the gut microbiota that are not positive.
Focus on establishing good sleep hygiene, such as getting to bed at the same time every night, shutting down screen time after a certain hour, and keeping the room you sleep in at a comfortable yet cool temperature.
If you want to find out more about sleep and how the prebiotic nature of Gut Performance™ enhances sleep, look at this blog post.
Stabilise your blood sugars
There is a lot of information out there about blood sugars and insulin. Some of its old thinking, some of it new and not yet proven. You need to remember that the more times you eat, with the higher concentration of carbs, the more likely you are going to force your blood sugar levels to rise.
Remember to keep processed carbohydrates such as white breads, pastas and sugars to a minimum and always pair your carbohydrates with a good fat and protein. Ensure to also add in both soluble and insoluble fibre (this is found largely in your green veggies and just quietly Gut Performance™). This will reign in the spikes in blood sugar levels.
Also – we are most insulin resistant after a fast and our first meal sets our blood sugar levels for 24 hours. Make sure your first meal is lower sugar and if you are having carbohydrates, pair these with a good fat and protein!
Fermented Foods
These foods have been used for centuries to heal and support gut health and the immune system. Include a dose of natural probiotics daily. These are foods such as kimchi, miso, kombucha (watch out for sugar), and pot fermented yogurt – if you are having dairy yoghurt, opt for full fat if your digestion allows to reduce glucose spikes.
Cruciferous Vegetables
If your diet is devoid of leafy greens, you need to stock up your shopping trolley the next time you are at the market. Kale, cauliflower, broccoli, and cabbage help support healthy elimination and regulate hormone balance in the gut. Remember to slightly cook these first (apart from cabbage) in order for our thyroid to stay happy!
The Bottom Line
PCOS is closely linked to an imbalanced gut microbiome. Your microbiota needs the right bacteria in the right amount to perform its hormone regulating functions properly. When the type or number of bacteria gets disturbed by events such as stress, or poor diet, your gut can no longer accomplish its job.
Supporting your gut health is priority number one if you are suffering from this condition.
Let us know via our Instagram #gut_performance if you have tried Gut Performance™ or Gut Performance™ + Collagen to support your gut health and heal PCOS. We know you are out there.
References
Bednarska, S., & Siejka, A. (2017). The pathogenesis and treatment of polycystic ovary syndrome: What’s new? Advances in clinical and eperiemental medicine, 26(2), 359-367. Retrieved 2022, from https://doi.org/10.17219/acem/59380
Collden, H., Landin, A., Wallenius, V., Elebring, E., Fandriks, L., Nilsson, M. E., . . . Ohlsson, C. (2019). The gut microbiota is a major regulator of androgen metabolism in intestinal contents. American Journal of Physiology-Endocrinology and Metabolism, 317(6), E1182-E1192. Retrieved from https://journals.physiology.org/doi/full/10.1152/ajpendo.00338.2019
Guo, Y., Qi, Y., Yang, X., Zhao, L., Wen, S., Liu, Y., & Tang, L. (2016). Association between Polycystic Oveary Syndrome and Gut Microbiota. PloS one, 11(4). Retrieved from https://doi.org/10.1371/journal.pone.0153196
Pedro, J., Siakowska, M., Banaszewska, B., Pawelczyk, L., Duleba, A., Kelley, S., & Thackray, V. (2018). Gut Microbial Diverstiy in Women With Polycystic Ovary Syndrome Correlates with Hyperandrogenism. The Journal of Endocrinology & Metabolism, 103(4), 1502-1511. Retrieved from https://doi.org/10.1210/jc.2017-02153
Rowland, I., Gibson, G., Heinke, A., Scott, K., Swann, J., Thiele, I., & Tuohy, K. (2017). Gut Microbiota functions: metabolism of nutrients and other food components. European Journal of Nutrition. doi:doi:10.1007/s00394-017-1445-8
Ruiz-Ojeda, F. J., Plaza-Diaz, J., Saez-Lara, M. J., & Gil, A. (2019). Effects of Sweeteners on the Gut Microbiota: A Review of Experimental Studies and Clinical Trials. Advances in nutrition, 10(suppl 1), S31-S48. Retrieved 2022, from https://doi.org/10.1093/advances/nmy037
Torres, P. J., Siakowska, M., Banaszewska, B., Pawelczyk, L., Duleba, A. J., Kelley, S. T., & Thackray, V. G. (2018). Gut Microbial Diversity in Women With Polycystic Ovary Syndrome Correlates with Hyperandrogenism. The Journal of Clinical Endocrinology and Metabolism, 103(4), 1502-1511. Retrieved from https://doi.org/10.1210/jc.2017-02153
Tremellen, K., & Pearce, K. (2012). Dysbiosis of Gut Microbiota (DOGMA) – A novel Theory for the Developement of Polycystic Ovarian Syndrome. Medical Hypothese, 79, 104-112.
Yildiz, B. O., & Azziz, R. (2007). The adrenal and polycystic ovary syndrome. Reviews in endocrine & metabolic disorders, 8(4), 331342. Retrieved from https://doi.org/10.1007/s11154-007-9054-0